However, he is still unable to return to work because he is so ill and he is collecting 60% of his pay on short term disability and bills still continue to come in. He has to meet rent, make car payments, and today had to pay $178 to his primary care provider and $40 to his oxygen supply company. He is unsure how long his employer will continue his health insurance and is unsure of the transition to long them disability in another 2 weeks.
My question is this.
Is this any way to treat a Hero?
Hospitalizations in Connecticut are down to 270 today.
We are 94 days since our first confirmed case, we topped out at 1,972 hospitalized patients, and we are 20 days into phase one of our reopening.
Kaiser Health News published a good article about the 600+ U.S. Healthcare Workers have died.
https://khn.org/news/exclusive-investigation-nearly-600-and-counting-us-health-workers-have-died-of-covid-19/
This link are Q&As from the CDC. The 4th Question deals with why the CDC “still recommends the use of N95 or better in caring for a Covid positive our person under investigation.”
Sometimes I think we forget that this has always been the CDCs position and that Contingency and Crisis capacities did not change this guidance, they only allowed a TEMPORARY relaxation of the guidance due to supply shortages.
The page was updated on May 29.
“CDC’s guidance to use NIOSH-approved N95 disposable filtering facepiece or higher level respirators when providing care for patients with suspected or known COVID-19 is based on the current understanding of SARS-CoV-2 and related respiratory viruses.
Current data suggest that close-range aerosol transmission by droplet and inhalation, and contact followed by self-delivery to the eyes, nose, or mouth are likely routes of transmission. Long-range aerosol transmission, such as is seen with measles, has not been a feature of SARS-CoV-2.
Potential routes of close-range transmission include splashes and sprays of infectious material onto mucous membranes and inhalation of infectious virions exhaled by an infected person. The relative contribution of each of these is not known for SARS-Co-V-2.
Facemasks commonly used during surgical procedures will provide barrier protection against droplet sprays contacting mucous membranes of the nose and mouth, but they are not designed to protect wearers from inhaling small particles. N95 and higher level respirators, such as other disposable filtering facepiece respirators, powered air-purifying respirators (PAPRs), and elastomeric respirators, provide both barrier and respiratory protection because of their tight fit and filtration characteristics.
Respirators should be used as part of a respiratory protection program that provides staff with medical evaluations, training, and fit testing.
Although facemasks are routinely used for the care of patients with common viral respiratory infections, N95 or higher level respirators are routinely recommended for emerging pathogens like SARS CoV-2, which have the potential for transmission via small particles, the ability to cause severe infections, and no specific treatments or vaccines.
CDC recommendations acknowledge the current challenges with limited supplies of N95s and other respirators. Facilities that do not have sufficient supplies of N95s and other respirators for all patient care should prioritize their use for activities and procedures that pose high risks of generating infectious aerosols and use facemasks for care that does not involve those activities or procedures. Detailed strategies for optimizing the supply of N95 respirators are available on the CDC website. Once availability of supplies is reestablished, the guidance states that the use of N95 and higher level respirators should resume.”
Failure to return as soon as possible to Conventional Capacity strategy (including N95 or better for Covid positive and PUI patients) increases the risk to the public and caregivers.
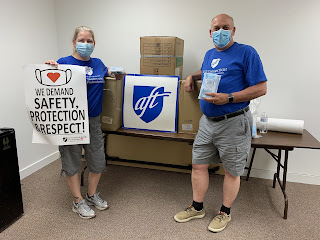
Today we delivered needed PPE to the Heroes of Windham and Natchaug Hospitals. The PPE was provided by the AFT Executive Committee under the leadership of President Randi Weingarten. (Jan sits on the Executive Committee)
We cannot thank the Executive Committee enough for their concern and solidarity with the healthcare workers of AFT.
Be well,
John

No comments:
Post a Comment